Cartilage injuries
- Home
- Treatments
- Cartilage injuries
Cartilage injuries
The articular cartilage is a thin layer of an elastic, resilient and very sliding structure that covers the joint surface. It allows the mobility of the joint and transmits the load through the articulation with a very low friction between the articular surfaces.
The cartilage injury is called chondropathy, and depending on the depth of the injury it is classified in several grades. When the injury also affects the bone below the cartilage it is called an osteochondral lesion. There is another kind of injury, the osteonecrosis or bone necrosis, where, after a sudden interruption of the blood supply to a part of the joint, a bone infarct occurs, and thus the affected bone area dies. It can progress either towards the healing of the area after some weeks or towards the definitive degeneration and damage of the articular cartilage.
Frequently, the cartilage injury occurs concurrently with other knee injuries, like the anterior cruciate ligament (ACL) tear, patellar dislocation or meniscal injuries. In these cases all of the injuries must be treated together.
The lack of articular cartilage reduces its cushioning effect, and so the direct load transmission to the bone produces pain. It can also produce swelling and knee locking, mostly when a cartilage fragment detaches and remains free in the joint, becoming a loose body. In these cases the patient feels that “something” is moving freely around their knee. This is also called “joint mouse”.
The diagnosis is confirmed by radiographs and magnetic resonance imaging (MRI).

The treatment depends on the grade of the injury (depth of the damage), its size and the location in the knee. For minor grades, restricted weight bearing is indicated, while full mobility of the knee is encouraged until the bone edema heals and the pain goes away. If after this conservative treatment some symptoms remain, an arthroscopy may be necessary to remove any small loose fragments that may be blocking the joint.
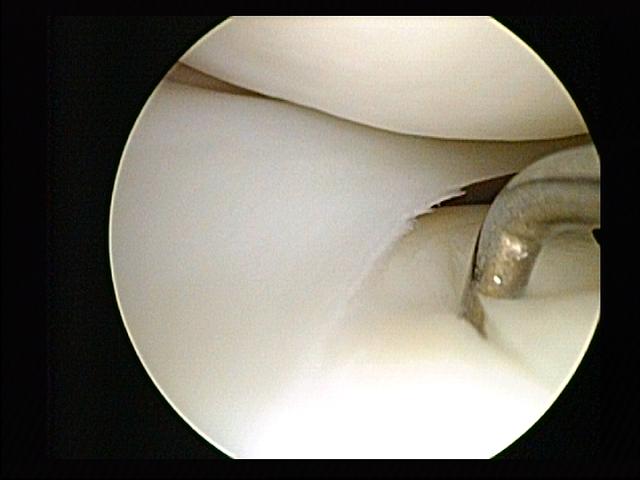
For severe grades, when the defect is deep and there is no cartilage on the lesion, an attempt to fill the defect must be made. Normally, it can be performed by arthroscopy, unless the extent of the injury makes an open procedure necessary.
When the chondral lesion is small we use a technique called microcfractures, in which millimetric fractures are made on the bed of the defect in order to stimulate the blood supply to the area and to create a fibrocartilaginous scar that fills the defect. The quality of the created layer is not the same as the original cartilage’s, but it can act in a similar way and the symptoms can be healed.
When the size of the lesion is quite large, we perform a technique of osteochondral autografting, called mosaicplasty. In this technique, small bone-cartilage cylinders are obtained from a non affected area of the knee in order to be transplanted in the chondral lesion, forming something similar to a mosaic, until almost the entire lesion is covered. The cylinders are obtained from a non bearing zone of the knee, so no additional damage is made after their harvest.
In all of the techniques mentioned above we usually add platelet-rich plasma injections, which brings growth factors and helps in the healing.
In postoperative care it is essential to avoid weight bearing for four to six weeks, while full mobility of the joint is encouraged. The patient can resume their normal life after three to six months, depending on the initial grade of the lesion.
When the cartilage damage is very large and it affects many areas of the knee, it is most likely an osteoarthritis. In this case, the above described treatments are not effective, and another solution must be offered (injections, osteotomies, knee replacement).

